Osteoporosis is a bone disease that weakens the bones, making them more prone to fractures. It is often called the “silent disease” because it can progress without any obvious symptoms until a bone breaks. Osteoporosis is a major health concern worldwide, affecting millions of people, particularly older adults. The condition occurs when the body loses too much bone mass or doesn’t make enough new bone to maintain a strong and healthy skeleton.
Understanding the risk factors, recognizing the symptoms, and knowing the effective strategies for prevention and management of osteoporosis are crucial in reducing the risk of fractures and improving quality of life. This article will dive into these areas to give you a comprehensive overview of osteoporosis, its prevention, and how it can be managed.

Table of Contents
- Introduction: What is Osteoporosis?
- Understanding the Causes and Risk Factors of Osteoporosis
- Symptoms of Osteoporosis
- Diagnosing Osteoporosis
- Preventive Strategies for Osteoporosis
- Management and Treatment Options for Osteoporosis
- Conclusion: Living with Osteoporosis
Introduction: What is Osteoporosis?
Osteoporosis is a medical condition where bones become fragile and brittle due to the loss of bone density. The term “osteoporosis” comes from Greek words meaning “porous bones.” The disease makes bones more vulnerable to fractures, especially in the spine, hips, and wrists. Over time, the bones lose their strength, making them more susceptible to breaking even with minor injuries or falls.
Although osteoporosis is commonly associated with aging, it can affect people at any age. It’s particularly prevalent in postmenopausal women, but it can affect both men and women. Understanding osteoporosis, its risk factors, and ways to manage and prevent it can help individuals avoid its severe consequences.
Understanding the Causes and Risk Factors of Osteoporosis
The causes of osteoporosis can be multi-faceted, involving genetic factors, lifestyle choices, and other health conditions. Let’s take a closer look at the most common risk factors.
2.1 Age and Gender
As people age, bone density naturally decreases. Women are at a higher risk of osteoporosis, particularly after menopause, due to a decrease in estrogen, a hormone that helps protect bones. While both men and women can develop osteoporosis, women are more likely to experience the condition due to hormonal changes that accelerate bone loss.
2.2 Family History and Genetics
A family history of osteoporosis can increase the risk of developing the condition. If a parent or sibling has had osteoporosis or fractures, there is a higher likelihood of developing bone-related problems. Genetics play a significant role in how bone mass is maintained throughout life.
2.3 Dietary Factors
A diet low in calcium and vitamin D can significantly increase the risk of osteoporosis. These nutrients are essential for maintaining healthy bone structure. Calcium is a major building block of bones, and vitamin D helps the body absorb calcium. Lack of these vital nutrients can result in brittle bones over time.
2.4 Lifestyle Factors
Certain lifestyle habits can contribute to the development of osteoporosis:
- Smoking: Smoking reduces blood flow to the bones and impairs calcium absorption.
- Alcohol: Excessive alcohol consumption can decrease bone density and interfere with the body’s ability to produce new bone.
- Sedentary lifestyle: Lack of weight-bearing physical activities such as walking or strength training can lead to bone loss.
2.5 Other Medical Conditions and Medications
Certain medical conditions, such as rheumatoid arthritis, thyroid disorders, and gastrointestinal diseases, can contribute to bone loss. Additionally, long-term use of medications like corticosteroids, proton pump inhibitors, and certain anticonvulsants can weaken bones.
Symptoms of Osteoporosis
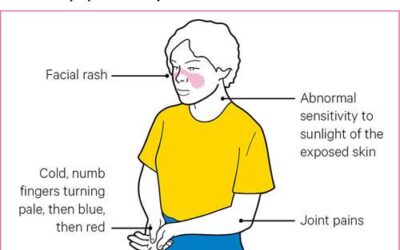
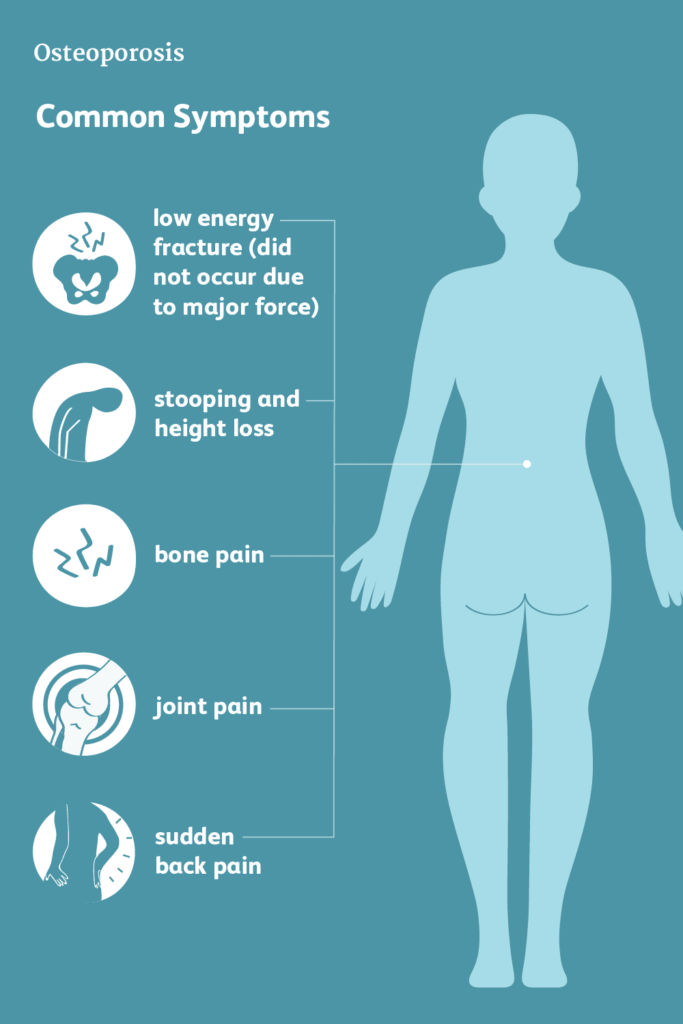
Osteoporosis often progresses without noticeable symptoms in the early stages. Many people are unaware they have the condition until a fracture occurs. However, some warning signs can suggest the presence of osteoporosis, including:
- Back pain: Due to a vertebral fracture or collapsed spine.
- Height loss: A decrease in height over time can be a sign of spinal fractures.
- Fractures: Bone fractures, especially in the hip, spine, or wrist, can occur with minimal or no trauma.
- Stooped posture: The spine may curve forward, leading to a hunched posture, a condition known as kyphosis.
Because osteoporosis is often asymptomatic, regular bone density testing and awareness of risk factors are crucial for early detection.
Diagnosing Osteoporosis
To diagnose osteoporosis, a doctor may perform several tests, including:
- Bone Mineral Density (BMD) Test: The most common method is dual-energy x-ray absorptiometry (DXA or DEXA), which measures bone density in the spine, hip, and forearm.
- X-rays: An X-ray may help detect fractures, especially if there’s an unexplained bone pain or height loss.
- Blood and Urine Tests: These tests help rule out other conditions that may affect bone health, such as hormonal imbalances or kidney disease.
Preventive Strategies for Osteoporosis
Preventing osteoporosis requires a combination of good lifestyle choices and nutritional habits.
5.1 Dietary Adjustments
A calcium-rich diet is essential to maintain bone density. Foods like dairy products, leafy greens, fortified plant-based milk, and fish with bones (like sardines) are excellent sources of calcium. Vitamin D is equally important and can be found in fortified foods, egg yolks, and exposure to sunlight.
5.2 Exercise and Physical Activity
Weight-bearing exercises, such as walking, jogging, hiking, and dancing, are excellent for strengthening bones. Resistance exercises that build muscle, like lifting weights or using resistance bands, can also help prevent bone loss and improve balance, reducing the risk of falls.
5.3 Vitamin and Mineral Supplements
If dietary intake is insufficient, supplements may be recommended. Calcium and vitamin D are particularly important for bone health. The recommended daily intake for calcium varies by age, but most adults need about 1,000-1,200 mg of calcium daily. Vitamin D helps the body absorb calcium and should be taken in adequate amounts.
Management and Treatment Options for Osteoporosis
For individuals who have been diagnosed with osteoporosis, treatment and management strategies can help strengthen bones, reduce fractures, and maintain quality of life.
6.1 Medications for Osteoporosis
Several medications are available to treat osteoporosis, including:
- Bisphosphonates (e.g., alendronate, ibandronate): These drugs help prevent bone breakdown and reduce the risk of fractures.
- Selective Estrogen Receptor Modulators (SERMs): These can mimic estrogen’s bone-protective effects and are mainly used for postmenopausal women.
- Denosumab: A monoclonal antibody that helps prevent bone resorption.
- Hormone Replacement Therapy (HRT): Sometimes used for women in menopause, though it carries risks.
6.2 Lifestyle Modifications
Making lifestyle changes can significantly reduce the risk of fractures and improve bone health:
- Quit smoking and limit alcohol: These habits are linked to bone loss.
- Fall prevention strategies: Home modifications, such as removing tripping hazards, using non-slip rugs, and adding grab bars in bathrooms, can prevent falls and fractures.
6.3 Physical Therapy
Physical therapy helps improve strength, flexibility, and balance. Specialized exercises can enhance bone density and reduce the risk of falls, especially for older individuals who may experience mobility issues.
Conclusion: Living with Osteoporosis
Osteoporosis is a serious condition that requires proactive management. While it’s impossible to reverse bone loss completely, the right combination of diet, exercise, and medical treatments can significantly reduce the risk of fractures and improve quality of life. By understanding the risk factors, recognizing symptoms, and taking preventive actions, individuals can better manage their bone health as they age.
If you suspect you may have osteoporosis or are at risk, consult your healthcare provider for a comprehensive evaluation and tailored treatment plan. Early intervention is key to living well with osteoporosis and maintaining strong, healthy bones.