Osteoporosis is a condition characterized by weakened bones that are more susceptible to fractures, particularly in older adults. It is one of the most common diseases affecting seniors, especially women, and it can lead to debilitating fractures, reduced mobility, and a lower quality of life. Understanding osteoporosis, its risk factors, and effective strategies for prevention and management can help seniors maintain their bone health and reduce the risk of fractures.
In this article, we will explore the causes and risk factors of osteoporosis, its symptoms, and the latest strategies for preventing bone fractures and promoting bone health in seniors.
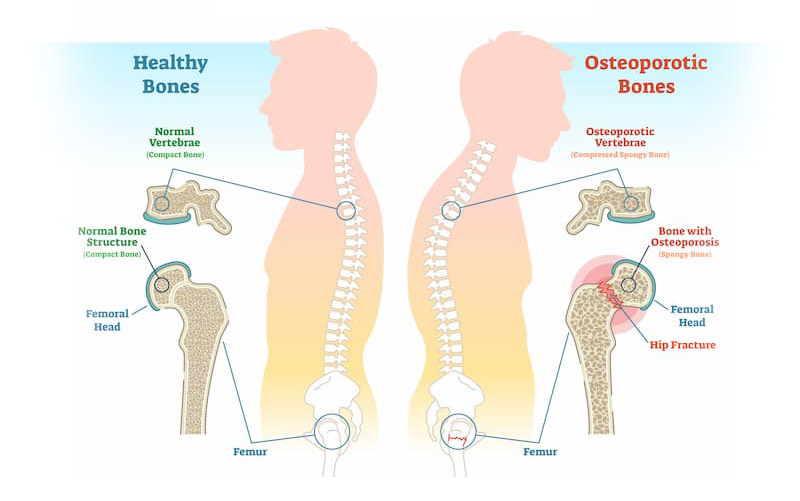
Table of Contents
- What is Osteoporosis?
- Risk Factors for Osteoporosis in Seniors
- Symptoms of Osteoporosis
- How is Osteoporosis Diagnosed?
- Preventing Osteoporosis and Bone Fractures
- Managing Osteoporosis: Treatment Options
- The Role of Physical Therapy in Osteoporosis
- Living with Osteoporosis: Tips for Seniors
- Conclusion: Empowering Seniors to Protect Their Bones
What is Osteoporosis?
Osteoporosis is a condition that causes bones to become weak, brittle, and more prone to fractures. It often develops slowly over many years, without symptoms in the early stages. As bones become thinner and more fragile, even a minor fall or bump can result in a broken bone. In severe cases, bones can fracture even without any trauma.
The most commonly affected bones in seniors are the spine, hips, and wrists. Osteoporosis can lead to decreased mobility, chronic pain, and even disability in older adults. Early intervention and effective management can help prevent fractures and maintain a higher quality of life for seniors.
Risk Factors for Osteoporosis in Seniors
Several risk factors can increase the likelihood of developing osteoporosis in seniors. While some of these factors are uncontrollable, others can be managed with lifestyle changes and proper care.
1. Age and Gender
The risk of osteoporosis increases with age, particularly in women over 50. Women are more likely to develop osteoporosis due to the decrease in estrogen levels during menopause, which plays a significant role in bone density.
2. Family History
A family history of osteoporosis or fractures can increase the risk of developing the disease. If parents or siblings have had osteoporosis or bone fractures, seniors may be at a higher risk.
3. Low Calcium and Vitamin D Intake
Calcium is essential for maintaining strong bones, while vitamin D helps the body absorb calcium. Seniors who do not get enough calcium or vitamin D through their diet or supplementation may be at higher risk for osteoporosis.
4. Sedentary Lifestyle
Physical activity is crucial for maintaining bone density. Lack of weight-bearing exercise, such as walking, dancing, or strength training, can contribute to bone weakening.
5. Smoking and Excessive Alcohol Consumption
Smoking and excessive alcohol consumption can interfere with the body’s ability to absorb calcium, impair bone formation, and increase the risk of osteoporosis.
6. Medical Conditions and Medications
Certain medical conditions, such as rheumatoid arthritis, hyperthyroidism, and chronic kidney disease, can increase the risk of osteoporosis. Additionally, long-term use of medications like corticosteroids, anticonvulsants, and certain cancer treatments can contribute to bone loss.
Symptoms of Osteoporosis
Osteoporosis is often called a “silent disease” because it may not show symptoms until a fracture occurs. However, some signs that may indicate the presence of osteoporosis include:
1. Back Pain
Chronic back pain, especially after lifting or bending, may be caused by a vertebral fracture due to weakened bones in the spine.
2. Loss of Height
Compression fractures in the spine can cause a gradual loss of height in individuals with osteoporosis.
3. Stooped Posture
Osteoporosis-related fractures in the spine can result in a hunched or stooped posture.
4. Easy Fractures
Bone fractures that occur from minor falls or everyday activities may be an early indication of osteoporosis.
How is Osteoporosis Diagnosed?
Osteoporosis is often diagnosed using a combination of medical history, physical exams, and diagnostic tests.
1. Bone Mineral Density (BMD) Test
The Dual-Energy X-ray Absorptiometry (DEXA) scan is the most common and reliable test to measure bone density. This test helps determine the risk of fractures and diagnose osteoporosis.
2. X-rays
X-rays may be used to identify fractures or bone damage, particularly in the spine, hips, and wrists.
3. Blood and Urine Tests
Blood and urine tests may help identify underlying conditions contributing to bone loss, such as thyroid disorders or vitamin D deficiencies.
Preventing Osteoporosis and Bone Fractures
Prevention is key when it comes to osteoporosis, as the condition is often difficult to reverse once it progresses. There are several lifestyle changes that can help prevent osteoporosis and maintain bone health in seniors.
5.1 Dietary Considerations for Bone Health
A balanced diet is essential for maintaining bone density. Seniors should focus on:
- Calcium-rich foods: Include dairy products, leafy green vegetables, fortified plant-based milks, and tofu in the diet.
- Vitamin D: Vitamin D helps the body absorb calcium. Sunlight exposure, fortified foods, and supplements can help seniors maintain adequate levels of vitamin D.
- Protein: Adequate protein intake supports bone health by promoting the production of collagen, which is a key component of bone structure.
5.2 Exercise for Osteoporosis Prevention
Regular physical activity helps maintain bone strength and reduce the risk of falls. Weight-bearing exercises, such as walking, hiking, and dancing, along with strength training, can improve bone density. Balance exercises, like tai chi or yoga, can also help prevent falls and fractures.
5.3 Lifestyle Changes to Improve Bone Health
In addition to diet and exercise, the following lifestyle changes can benefit bone health:
- Quit smoking: Smoking impairs bone health by reducing blood flow to the bones and decreasing calcium absorption.
- Limit alcohol: Excessive alcohol consumption can weaken bones and interfere with bone formation.
- Fall-proof your home: Installing grab bars, using non-slip mats, and keeping the home well-lit can help prevent falls in seniors with osteoporosis.
Managing Osteoporosis: Treatment Options
While osteoporosis cannot be fully cured, there are various treatments that can help manage the condition, prevent fractures, and improve the quality of life for seniors.
6.1 Medications for Osteoporosis
Several medications can help prevent bone loss and reduce the risk of fractures. Some commonly prescribed medications include:
- Bisphosphonates: Medications like alendronate (Fosamax) and ibandronate (Boniva) slow bone loss and can help prevent fractures.
- Hormone Replacement Therapy (HRT): In postmenopausal women, HRT may help maintain bone density.
- Denosumab (Prolia): This medication is a monoclonal antibody that can help slow bone loss.
- Teriparatide (Forteo): This synthetic form of parathyroid hormone stimulates bone formation.
6.2 Non-Pharmacological Treatments
Non-drug treatments like physical therapy, nutrition counseling, and fall prevention strategies are also critical components of osteoporosis management.
The Role of Physical Therapy in Osteoporosis
Physical therapy plays a crucial role in managing osteoporosis. A physical therapist can design an individualized exercise program that targets bone strengthening, improves balance, and reduces the risk of falls. Safe exercises such as stretching, weight-bearing activities, and core strengthening exercises can help maintain mobility and independence in seniors with osteoporosis.

Living with Osteoporosis: Tips for Seniors
Managing osteoporosis requires consistent attention to lifestyle choices and treatments. Here are some tips for seniors living with osteoporosis:
- Follow your treatment plan: Adhere to medications and physical therapy recommendations as prescribed by your healthcare provider.
- Get regular check-ups: Monitor bone density through regular DEXA scans to assess progress.
- Stay active: Engage in weight-bearing and balance exercises regularly.
- Prioritize bone-healthy foods: Incorporate calcium and vitamin D-rich foods into your diet.
Conclusion: Empowering Seniors to Protect Their Bones
Osteoporosis is a manageable condition, and with the right lifestyle choices, treatment options, and prevention strategies, seniors can protect their bones and reduce the risk of fractures. By focusing on a healthy diet, regular exercise, medication when necessary, and fall prevention, seniors can maintain their bone health and continue to lead active, independent lives.