Introduction
Type 2 diabetes is a chronic condition that affects millions of people worldwide. As a leading cause of complications such as heart disease, kidney failure, and nerve damage, early diagnosis and proper management are essential. Family physicians play a crucial role in providing comprehensive care by addressing lifestyle changes, medication management, and emotional well-being. This article explores a holistic approach to managing Type 2 diabetes in family medicine.
Understanding Type 2 Diabetes
Type 2 diabetes occurs when the body becomes resistant to insulin or when the pancreas fails to produce enough insulin to regulate blood sugar levels effectively. Unlike Type 1 diabetes, which is an autoimmune condition, Type 2 diabetes is primarily influenced by lifestyle factors, genetics, and metabolic health.
Risk Factors and Causes
Several factors contribute to the development of Type 2 diabetes:
- Genetics: Family history increases susceptibility.
- Obesity: Excess body weight, especially abdominal fat, raises insulin resistance.
- Sedentary Lifestyle: Lack of physical activity contributes to poor glucose metabolism.
- Unhealthy Diet: High intake of processed foods, sugars, and unhealthy fats leads to insulin resistance.
- High Blood Pressure & Cholesterol: These conditions often coexist with diabetes.
- Age: The risk increases after age 45.
- Ethnicity: Certain ethnic groups, including African Americans, Hispanics, and Asians, have a higher predisposition.
Symptoms and Early Warning Signs
Type 2 diabetes symptoms often develop gradually and may include:
- Increased thirst and frequent urination
- Unexplained weight loss
- Fatigue and irritability
- Blurred vision
- Slow-healing wounds
- Frequent infections
- Tingling or numbness in hands and feet
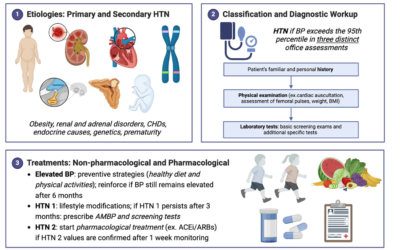
Diagnosis and Screening in Primary Care
Family physicians use several tests to diagnose diabetes:
| Test | Normal Range | Pre-Diabetes | Diabetes Diagnosis |
|---|---|---|---|
| Fasting Blood Sugar | <100 mg/dL | 100-125 mg/dL | ≥126 mg/dL |
| HbA1c (3-month avg) | <5.7% | 5.7-6.4% | ≥6.5% |
| Oral Glucose Tolerance Test | <140 mg/dL | 140-199 mg/dL | ≥200 mg/dL |
| Random Blood Sugar | – | – | ≥200 mg/dL with symptoms |
Treatment Approaches in Family Medicine
Managing Type 2 diabetes in a family medicine setting involves:
- Patient Education: Helping individuals understand diabetes and self-care strategies.
- Lifestyle Interventions: Encouraging diet and exercise modifications.
- Medication Management: Prescribing appropriate glucose-lowering drugs.
- Regular Monitoring: Tracking blood sugar, blood pressure, and cholesterol.
- Comprehensive Care: Addressing complications and coordinating with specialists when needed.
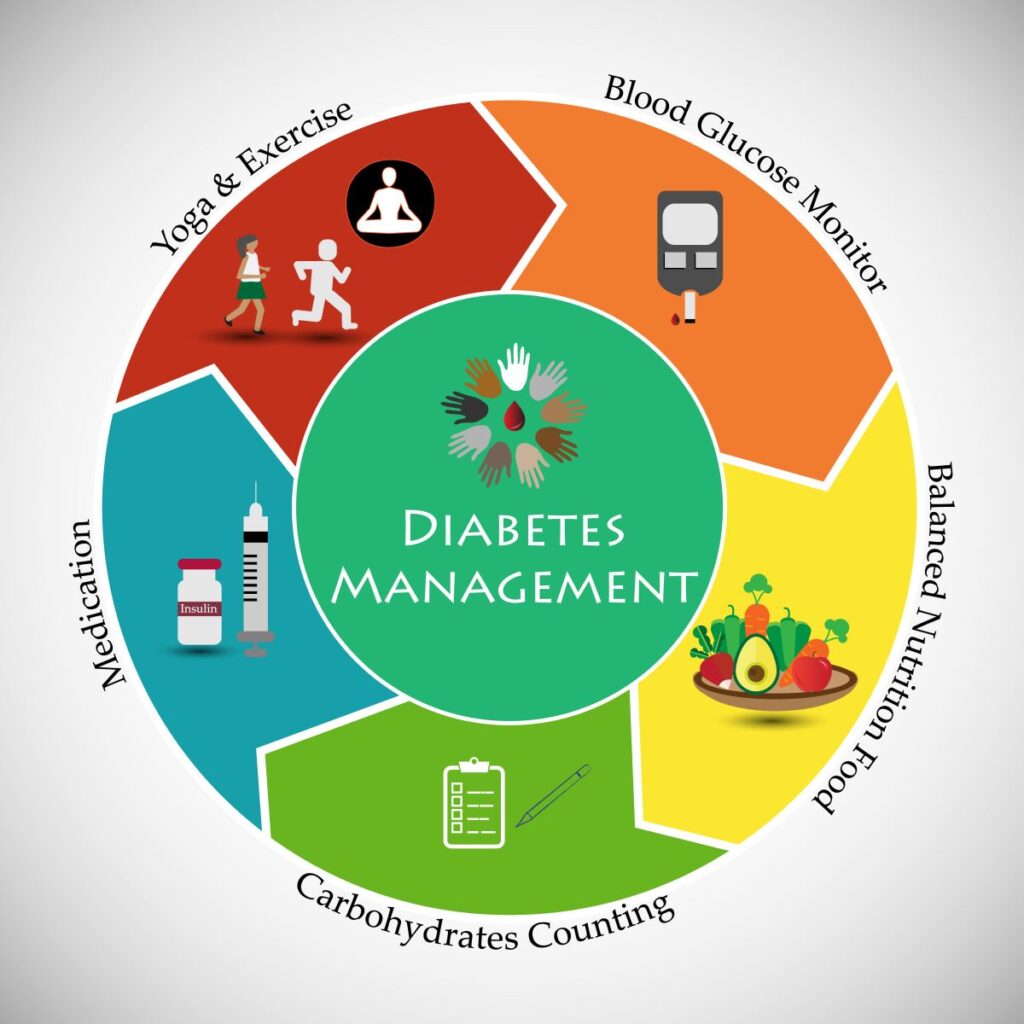
Lifestyle Modifications for Diabetes Management
1. Dietary Changes
- Adopt a balanced diet rich in whole grains, lean proteins, healthy fats, and fiber.
- Follow a low glycemic index (GI) diet to maintain stable blood sugar levels.
- Limit processed foods, added sugars, and refined carbohydrates.
- Increase intake of non-starchy vegetables like spinach, broccoli, and carrots.
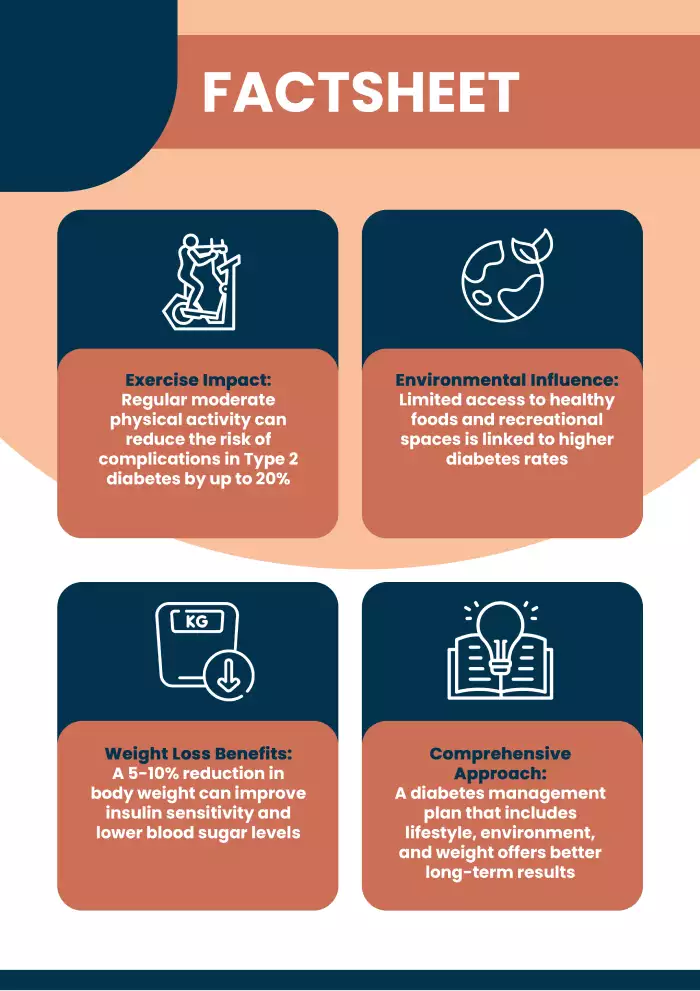
2. Physical Activity
- Engage in at least 150 minutes of moderate-intensity exercise per week.
- Include strength training exercises to improve insulin sensitivity.
- Simple activities like walking, swimming, and yoga can be beneficial.
3. Weight Management
- Losing 5-10% of body weight significantly improves blood sugar control.
- Avoid crash diets and focus on sustainable eating habits.
4. Sleep and Stress Management
- Poor sleep and chronic stress increase blood sugar levels.
- Practice mindfulness, meditation, and deep breathing exercises.
- Aim for 7-9 hours of quality sleep per night.
Medications and Insulin Therapy
Oral Medications
| Drug Class | Function | Examples |
| Metformin | Reduces liver glucose production | Glucophage |
| Sulfonylureas | Increases insulin release | Glipizide, Glyburide |
| SGLT2 Inhibitors | Enhances glucose excretion through urine | Empagliflozin, Dapagliflozin |
| DPP-4 Inhibitors | Helps regulate blood sugar levels | Sitagliptin, Linagliptin |
Insulin Therapy
- Required for some patients when oral medications are insufficient.
- Various types include rapid-acting, short-acting, intermediate, and long-acting insulin.
The Role of Mental Health in Diabetes Care
Managing Type 2 diabetes goes beyond physical health; mental well-being is also essential.
- Diabetes Burnout: Patients may feel overwhelmed and discouraged.
- Depression & Anxiety: Common in diabetes patients and can impact self-care.
- Support Groups & Counseling: Engaging in community or therapy can improve motivation and adherence to treatment.
Preventing Complications of Type 2 Diabetes
Proper management helps prevent complications such as:
- Cardiovascular Disease: Control blood pressure and cholesterol.
- Kidney Disease (Nephropathy): Regular kidney function tests are essential.
- Nerve Damage (Neuropathy): Monitor foot health and seek early treatment for tingling or numbness.
- Eye Disease (Retinopathy): Regular eye exams help prevent vision loss.
- Foot Ulcers & Infections: Daily foot care and proper footwear can prevent complications.
Conclusion
Managing Type 2 diabetes in family medicine requires a holistic approach that incorporates patient education, lifestyle modifications, medication management, and mental health support. Family physicians play a crucial role in helping individuals lead healthier lives by addressing all aspects of diabetes care. With the right interventions, patients can control their condition, reduce complications, and improve overall well-being.