Introduction
COVID-19 has triggered a worldwide pandemic that delivered severe consequences to humanity through its devastating impact on people collectively with societies and medical care organizations across the planet.
The pandemic mostly hit urban areas alongside healthcare systems but brought distinctive complications to closed group populations within nursing homes prisons military bases and similar congregational facilities.
The combination of restricted living spaces and constrained freedom with susceptible inhabitants caused these residential groups to fight against fast COVID-19 transmission during the pandemic and continue experiencing long-term health effects after recovery.
This article investigates COVID-19 transmission in closed communities before analyzing post-COVID impacts on these communities through mental health problems and healthcare system stresses and current public health requirements.
The Rise of COVID-19 in Closed Communities
Nursing homes together with prisons shelters and military bases have proven to be high-risk areas for infectious disease transmission of COVID-19.
Such living arrangements that position multiple people together prevent proper execution of social distancing plans and basic hygiene protocols.
The swift transmission of COVID-19 in these communities worsened the primary health emergency along with the extended impact it had on affected populations.
Factors Contributing to the Spread in Closed Communities
Residential premises provide multiple points for physical interaction among occupants and staff which makes it easy for viruses to spread rapidly.
Several closed communities maintain population segments composed of weakened individuals whose preexisting health issues such as old age and chronic illnesses make them susceptible to severe COVID-19 complications or death.
The lack of adequate protective equipment and testing capabilities and medical supplies created barriers in stopping outbreak spread in certain closed communities once infections began to emerge.
Social distancing protocols and testing protocols and patient isolation measures remained delayed throughout the initial virus spread because community leaders did not understand COVID-19 well enough.
The accelerating spread of COVID-19 within these communities generated high death rates most severely affecting senior people along with people with health problems.
Medical facilities confronted overwhelming infection numbers which depleted medical personnel and made proper patient care challenging and elevated mental stress levels.
Post-COVID Implications in Closed Communities
The acute emergency health threat of COVID-19 in confined residential communities seems to have diminished across many areas yet these populations face ongoing difficulties from COVID aftermaths.
The effects of COVID-19 persist into the future because people experience both medical complications combined with ongoing psychological issues in addition to life-changing disruptions and potential new outbreaks of coronavirus.
🔘 Mental Health Consequences
- Modern society has significantly harmed mental health for closed community members who were confined in their homes through lockdowns or quarantine periods. Social Isolation: Many residents of closed communities, especially the elderly, experienced extreme social isolation during lockdowns.
- Engaging with family became limited due to quarantine rules which resulted in social events being discontinued therefore people experienced loneliness and anxiety and depression.
- The anxiousness about getting COVID-19 and the unclear situation regarding the pathogen introduced significant pressure. People living in crowded residences experienced greater anxiety after the pandemic began. Daily life routines of several residents broke down leading to confusion and having no structure to follow.
- Elderly adults along with those who have cognitive impairment faced great challenges because they depend on consistency to maintain their well-being. Post-COVID Mental Health Support The necessary solution to treat mental health starts with effective actions in enclosed communities following COVID outbreaks.
- Several programs including counseling sessions over video conference and stress management applications together with better family-resident communication will assist in reducing psychological harm. Each community requires specialized mental health services for building emotional resilience and achieving recovery.
🔘 Healthcare Strain and Recovery Challenges
- Current healthcare facilities in closed communities face ongoing difficulties because of the pandemic effects. Several enduring medical care problems require immediate solutions.
- The residents who survived COVID-19 in closed communities face ongoing health problems after recovery that medical experts class as “long COVID.” Long COVID creates multiple health symptoms including extreme tiredness together with breathing problems and thinking problems which affect how people function every day.
- Healthcare staff members in confined communities reached their maximum tolerance levels during the pandemic and some professionals quit their positions because of stress combined with illness and deficient workplace support.
- The healthcare workforce shortage creates challenges for communities to maintain proper resident care when they fight to overcome pandemic-related difficulties. Closed community populations endure greater risk of future outbreaks because their densely populated areas along with easy disease transmission.
- The prevention of future health crises demands ready access to both adequate resources and prepared infrastructure along with response plans by the communities. Healthcare Solutions Moving Forward The proper development of healthcare systems inside closed communities requires substantial investments to equip them properly for future health emergencies.
- Medical systems must extend their support through better staff deployment and supply distribution with rapid testing capability development. Long COVID recovery monitoring and precise treatment provision for former COVID-19 patients must continue through ongoing residency-based support systems.
- Healthcare institutions must establish interconnected support systems that provide both physical therapy and mental health counseling services to long COVID patients.
🔘 Disruption to Daily Life and Activities
- A lengthy disruption of routine community activities throughout the pandemic generated negative consequences for the overall life quality of residents.
- The continuation of imposed pandemic restrictions on recreational freedom has persistently affected community life regardless of lifting these restrictions.
- Closed community residents depend on their regular social activities which include communal dining as well as communal activities and participation in religious services. Social restrictions caused social connection levels to decrease thus negatively affecting mental wellness of people.
- The pandemic has caused an expansion of personal attendance requirements particularly affecting elderly and vulnerable individuals.
- COVID-19 has triggered the necessity for enhanced care needs because it caused lasting health complications among multiple people.
Rebuilding Community Life Post-COVID
The recovery process of closed communities after COVID requires initiatives which aim to rebuild their traditional way of life.
The successful reintegration of community social activities and safe resident interaction combined with community participation initiatives will help transition people back to more connected lives.
Solutions and Strategies for Future Protection
Both present-day solutions and long-term strategies must be developed to improve safety conditions together with mental health and enhance total well-being in closed communities during COVID-19.
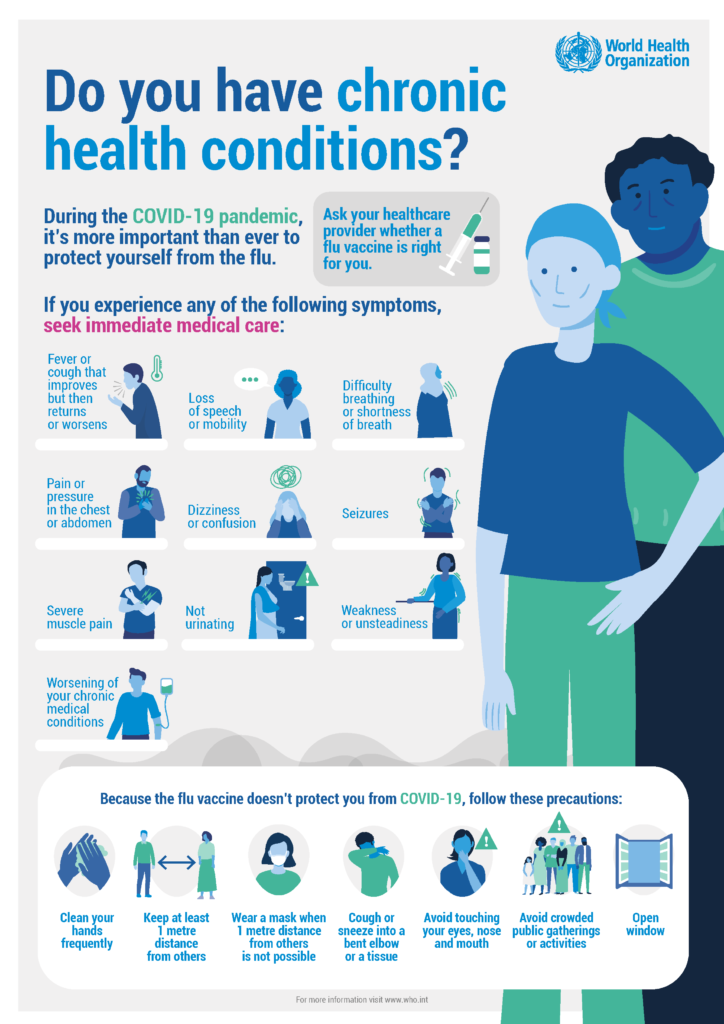
Some key strategies include: Health institutions should develop upgraded infection control protocols which combine regular testing with isolation protocols and vaccination programs to prevent future outbreak occurrences. Protocols should be kept current with ability to accommodate emerging virus variants.
Telemedicine enables patients to get healthcare remotely with no physical requirements thus lowering transmission risks. It is essential to extend telehealth capabilities to perform routine examinations and conduct mental health counseling and care for COVID-19 survivors.
Programs that develop resilience among residents and employees should be implemented because they function as essential tools for future infectious outbreaks.
Future crises will have reduced psychological impact on staff and residents through combined offering of stress management tools along with educational sessions and frequent information updates.
The establishment of updated infrastructure that provides better ventilation and sanitation and enables social distancing makes it possible to decrease infectious disease transmission within enclosed communities.
Distributing sufficient PPE materials along with establishing fast-acting healthcare teams represents priority measures.
Conclusion
Closed community environments now demonstrate clearly how vulnerable they remain against infectious diseases after the COVID-19 outbreak spread throughout such settings.
Multiple long-term impacts on well-being and healthcare services together with daily routines will ongoingly affect these communities because of the pandemic.
Through implementing proven public health protocols and mental health support systems and healthcare developments closed communities will develop into de facto resilient health systems for upcoming health emergencies.
The COVID-19 pandemic should be used to create guidelines for future policy that provides necessary tools and resources for maintaining safety in closed communities.