Lupus is a chronic autoimmune disease that can affect various parts of the body, including the skin, joints, kidneys, heart, and lungs. It occurs when the body’s immune system mistakenly attacks its own tissues and organs. This can lead to inflammation, pain, and damage in affected areas. Lupus is often referred to as a “complex” disease because its symptoms can vary greatly from person to person, and they may come and go in flare-ups.
While lupus can affect anyone, it is more common in women, particularly those of childbearing age. Early diagnosis and appropriate treatment are crucial for managing lupus and minimizing its impact on the quality of life.
In this article, we will explore the symptoms of lupus, how it is diagnosed, and the various treatment options available to manage this complex disease.
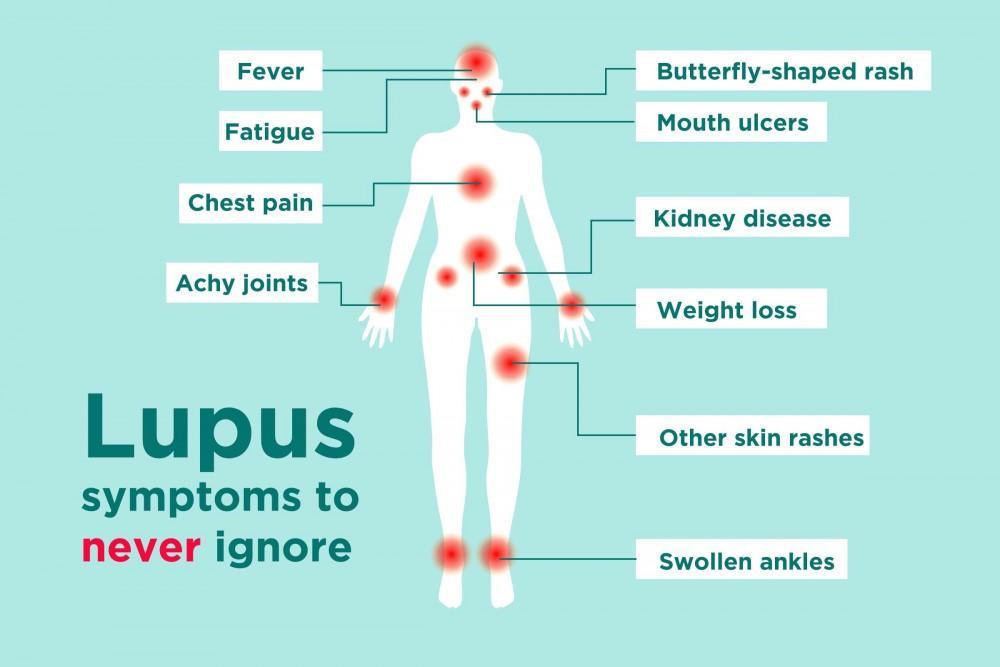
Table of Contents
- What is Lupus?
- Understanding the Causes and Risk Factors of Lupus
- Common Symptoms of Lupus
- How is Lupus Diagnosed?
- 4.1 Blood Tests
- 4.2 Imaging Tests
- 4.3 Biopsy
- Treatment Options for Lupus
- Managing Lupus Flares and Complications
- Living with Lupus: Tips for Patients
- Conclusion: Hope and Advancements in Lupus Research
What is Lupus?
Lupus is an autoimmune disease, meaning that the body’s immune system, which is designed to fight off infections, mistakenly attacks healthy tissues and organs. This leads to inflammation and damage in various parts of the body.
There are several forms of lupus, with the most common being systemic lupus erythematosus (SLE), which can affect multiple organs. Other forms include discoid lupus, which primarily affects the skin, and drug-induced lupus, which can be caused by certain medications.
The exact cause of lupus is unknown, but it is believed to result from a combination of genetic, environmental, and hormonal factors.
Understanding the Causes and Risk Factors of Lupus
Lupus is a complex disease, and the exact cause is still not fully understood. However, certain risk factors can make a person more likely to develop lupus:
Genetics
Family history plays a significant role in lupus. People with close relatives who have lupus or other autoimmune diseases are at a higher risk of developing the disease. Certain genetic factors may predispose individuals to the condition.
Hormonal Factors
Lupus is more common in women, particularly those between the ages of 15 and 45. This suggests that hormonal changes, especially related to estrogen, may play a role in the development of lupus. Many women experience flare-ups of lupus symptoms during pregnancy or when taking oral contraceptives.
Environmental Triggers
Certain environmental factors are believed to trigger lupus in individuals with a genetic predisposition. These factors can include:
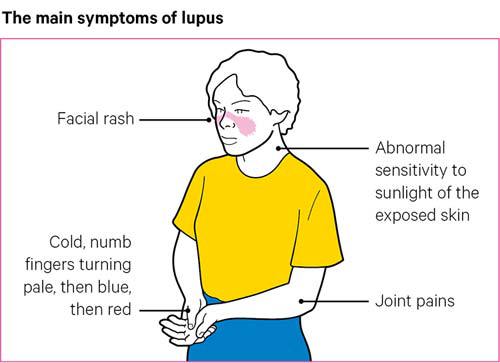
- Sunlight exposure: Ultraviolet (UV) rays from the sun can trigger lupus flares, particularly in people with skin involvement.
- Infections: Viral or bacterial infections may trigger lupus in genetically predisposed individuals.
- Medications: Certain medications, such as antibiotics and anticonvulsants, can cause drug-induced lupus, which usually resolves once the medication is stopped.
Ethnicity
Lupus is more common in certain ethnic groups, including African Americans, Hispanics, Asians, and Native Americans. These groups are more likely to develop severe forms of the disease.
Common Symptoms of Lupus
The symptoms of lupus can vary greatly depending on the individual, the type of lupus they have, and the organs involved. Some of the most common symptoms of lupus include:
1. Fatigue
Fatigue is one of the most common and debilitating symptoms of lupus. People with lupus often experience a lack of energy that can interfere with daily activities.
2. Joint Pain and Swelling
Lupus often causes inflammation in the joints, leading to pain, swelling, and stiffness, particularly in the hands, wrists, and knees.
3. Skin Rash
A distinctive butterfly-shaped rash that appears across the cheeks and nose is one of the hallmark signs of lupus. This rash can worsen with sun exposure, a condition known as photosensitivity.
4. Fever
Many people with lupus experience unexplained fevers, especially during disease flares.
5. Kidney Problems
Lupus can cause inflammation in the kidneys (lupus nephritis), which can lead to kidney damage. Symptoms of kidney problems may include swelling in the legs, ankles, or around the eyes.
6. Chest Pain and Difficulty Breathing
Inflammation of the lining around the heart or lungs can cause chest pain, shortness of breath, and difficulty breathing, particularly when taking a deep breath.
7. Mouth and Nose Ulcers
Painful ulcers may develop in the mouth or nose, often without any obvious cause.
How is Lupus Diagnosed?
Diagnosing lupus can be challenging because its symptoms mimic those of other diseases. There is no single test to confirm lupus, but a combination of blood tests, imaging studies, and clinical evaluation can help doctors make a diagnosis.
4.1 Blood Tests
The most common blood test used to diagnose lupus is the antinuclear antibody (ANA) test, which detects abnormal antibodies in the blood that attack the body’s cells. Other tests, such as the anti-dsDNA test, help confirm the diagnosis.
4.2 Imaging Tests
Imaging tests, such as X-rays or ultrasounds, may be used to assess organ damage or inflammation, especially in the kidneys or heart.
4.3 Biopsy
In some cases, a biopsy of the skin, kidneys, or other organs may be necessary to confirm lupus and determine the extent of organ damage.
Treatment Options for Lupus
While there is no cure for lupus, there are many treatment options to help manage the disease, reduce symptoms, and prevent organ damage. Treatment plans are highly individualized, depending on the severity of the disease and the organs involved.
5.1 Medications
The primary goal of lupus treatment is to control inflammation and suppress the immune system to prevent further damage. Medications commonly prescribed for lupus include:
- Nonsteroidal anti-inflammatory drugs (NSAIDs): For pain and inflammation.
- Antimalarial drugs: Hydroxychloroquine is often used to treat skin and joint symptoms of lupus.
- Corticosteroids: These medications reduce inflammation and control flare-ups.
- Immunosuppressive drugs: Drugs such as methotrexate and cyclophosphamide suppress the immune system and prevent organ damage in severe cases.
5.2 Lifestyle Modifications
Living with lupus requires careful lifestyle management. Patients are encouraged to:
- Avoid excessive sun exposure: Use sunscreen and wear protective clothing to prevent skin rashes.
- Exercise regularly: Low-impact exercises, like swimming or walking, can improve joint health and reduce fatigue.
- Manage stress: Stress can trigger flare-ups, so stress management techniques, such as yoga or meditation, are important.
5.3 Complementary Therapies
Some people with lupus benefit from complementary therapies such as acupuncture, massage therapy, or dietary supplements. It’s essential to consult a healthcare provider before trying any complementary treatments.
Managing Lupus Flares and Complications
Lupus is a disease that goes through periods of flare-ups, where symptoms worsen, and periods of remission, where symptoms improve. During a flare-up, it’s important to follow the prescribed treatment plan, rest, and avoid triggers. Regular check-ups and monitoring for complications such as kidney damage or cardiovascular disease are also important.
Living with Lupus: Tips for Patients
Living with lupus can be challenging, but with proper care and support, individuals can manage their symptoms and lead fulfilling lives. Here are some tips for those living with lupus:
- Stay informed: Understand your condition and work closely with your healthcare team.
- Support system: Seek emotional support from family, friends, or support groups.
- Be mindful of your health: Follow your treatment plan, get enough sleep, eat a healthy diet, and manage stress effectively.
Conclusion: Hope and Advancements in Lupus Research
Lupus remains a complex disease with no cure, but advancements in research and treatments offer hope for better management and quality of life for those living with the condition. By understanding the symptoms, getting early diagnosis, and pursuing appropriate treatment options, people with lupus can better manage their condition and lead healthier, happier lives.
With ongoing research and increasing awareness, the future for lupus patients looks promising. Early intervention, personalized treatments, and lifestyle changes can make a significant difference in managing this chronic autoimmune disease.

