Thymic carcinoma, a rare and aggressive cancer that forms in the thymus gland, has historically been difficult to treat, particularly in its advanced stages. Located just beneath the breastbone, the thymus plays a role in immune system development, making this cancer particularly complex. In recent years, new research has emerged, offering hope to patients with advanced thymic carcinoma through innovative treatment options.
In this article, we explore the promising advancements in therapies for thymic carcinoma, examining how novel treatments may extend survival and improve quality of life for those facing this challenging diagnosis.
Understanding Thymic Carcinoma
Thymic carcinoma is a form of cancer originating in the thymus, a small gland that produces T-cells, which are essential for the immune system. Unlike thymomas, which tend to grow slowly and are often confined to the thymus, thymic carcinoma is more aggressive, often spreading to nearby organs or distant parts of the body. The cancer’s rarity, affecting fewer than 1.5 per million people annually, has limited large-scale research and treatment development compared to other cancers.
Patients with thymic carcinoma frequently face challenges in diagnosis due to the cancer’s vague symptoms, such as chest pain, shortness of breath, or persistent cough, which can be mistaken for less severe conditions. By the time thymic carcinoma is detected, it is often in advanced stages, requiring more aggressive treatments.
Current Treatment Options and Their Limitations
Historically, treatment for thymic carcinoma has included surgery, radiation therapy, and chemotherapy, particularly for early-stage cases. Surgery to remove the tumor offers the best chance of cure if the cancer is detected early, but in many cases, the cancer is already too advanced to be surgically resected.
Chemotherapy has been the standard approach for advanced or unresectable thymic carcinoma. However, the results are often mixed, with many patients experiencing significant side effects and limited improvement in survival rates. Radiation therapy may also be used, but it typically serves as an adjunct treatment rather than a curative option.
In light of these limitations, there has been a growing interest in developing novel therapies for patients with advanced thymic carcinoma.
Promising New Treatment Option: Immunotherapy
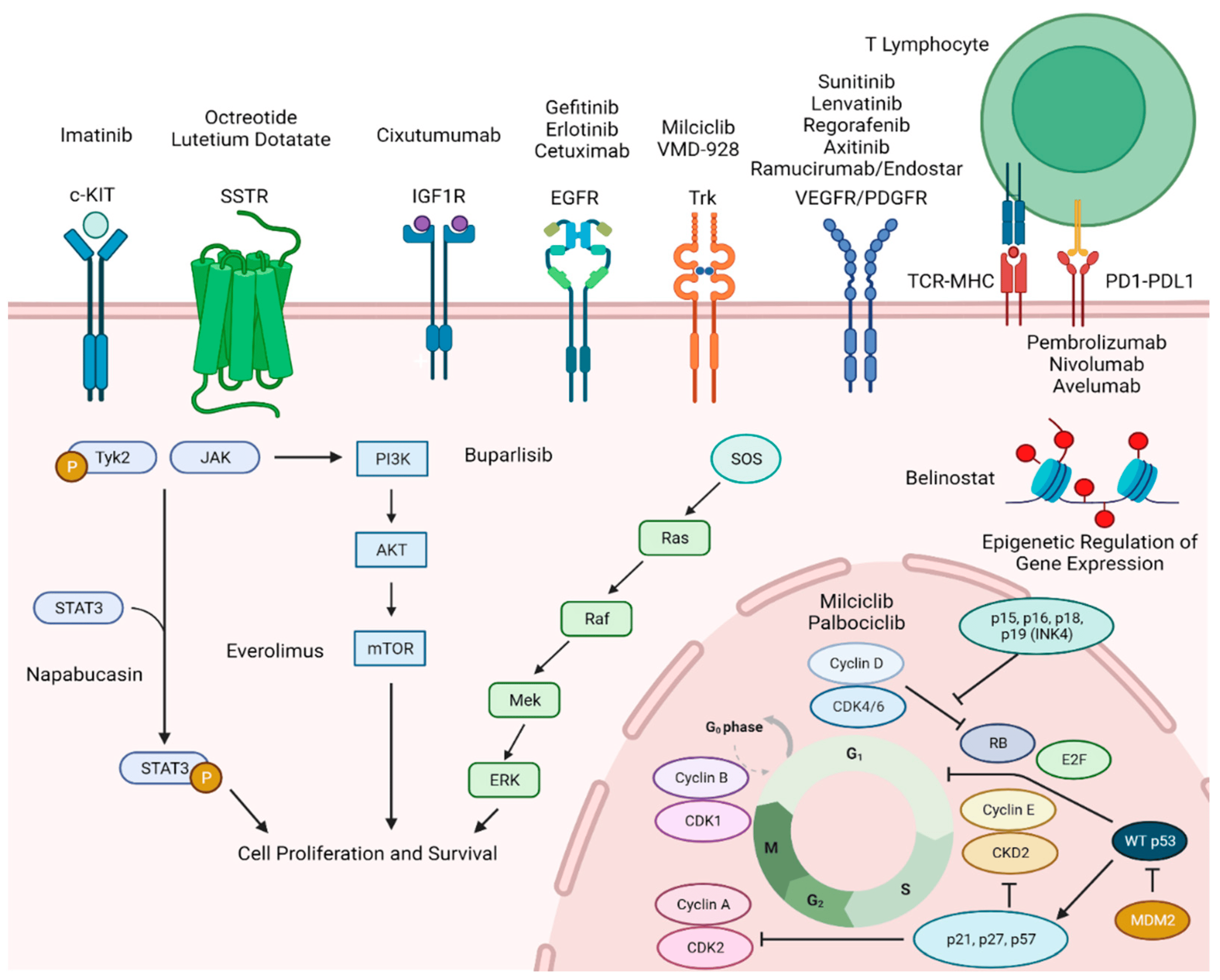
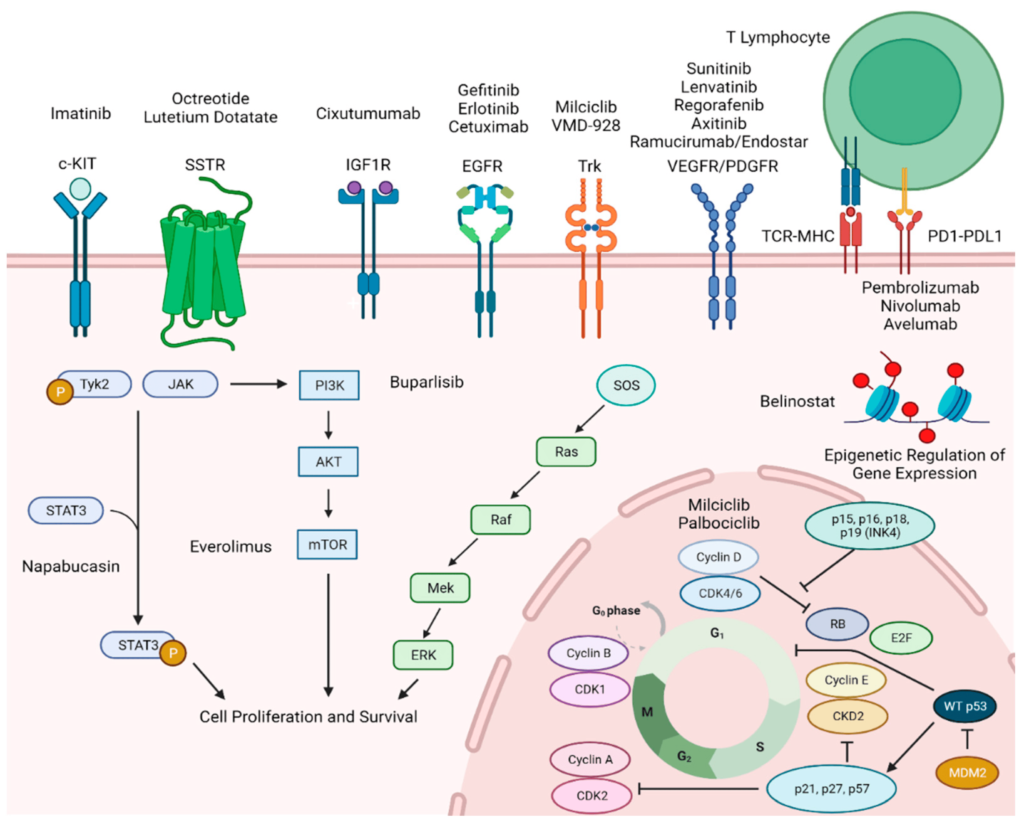
One of the most exciting developments in the treatment of advanced thymic carcinoma is immunotherapy, a class of treatments designed to harness the body’s immune system to attack cancer cells. Immunotherapy has already shown success in treating various other cancers, such as melanoma, lung cancer, and kidney cancer, but only recently has it been investigated as a potential therapy for thymic carcinoma.
A promising new study published in The Lancet Oncology revealed that a specific immunotherapy drug, pembrolizumab (marketed as Keytruda), may offer hope to patients with advanced thymic carcinoma. Pembrolizumab is a type of immune checkpoint inhibitor that blocks a protein called PD-1, which cancer cells often use to avoid detection by the immune system. By inhibiting this protein, pembrolizumab allows the immune system to recognize and destroy cancer cells more effectively.
In a clinical trial, researchers found that pembrolizumab helped shrink tumors in approximately 22% of patients with advanced thymic carcinoma, with some individuals showing durable responses lasting over two years. Importantly, the treatment appeared to stabilize disease progression in a significant number of patients, even if complete tumor shrinkage was not achieved.
Benefits and Challenges of Immunotherapy
Immunotherapy offers several potential benefits for patients with advanced thymic carcinoma. For one, it provides an option for those who have exhausted conventional treatments like chemotherapy and radiation. Additionally, immunotherapy tends to have fewer severe side effects compared to traditional chemotherapy, which can significantly improve patients’ quality of life during treatment.
However, there are also challenges and risks associated with immunotherapy. While the results are promising, not all patients respond to treatment, and researchers are still working to identify biomarkers that predict who will benefit the most from immunotherapy. Additionally, because immunotherapy activates the immune system, there is a risk of developing autoimmune-like side effects, such as inflammation of the lungs or liver, which can be serious in some cases.
Ongoing Research and Future Prospects
The development of immunotherapy represents a crucial step forward for advanced thymic carcinoma, but more research is needed to fully understand its potential. Ongoing clinical trials are investigating the use of pembrolizumab in combination with other treatments, such as chemotherapy or radiation, to determine if these approaches can enhance the effectiveness of immunotherapy.
Researchers are also exploring other immunotherapy drugs that target different pathways in the immune system, aiming to expand treatment options for patients who do not respond to PD-1 inhibitors like pembrolizumab. Additionally, advances in personalized medicine, which tailors treatment to the genetic makeup of an individual’s tumor, may further refine and improve treatment strategies for thymic carcinoma in the future.
Conclusion
The emergence of immunotherapy as a potential treatment for advanced thymic carcinoma marks a significant milestone in the fight against this rare and aggressive cancer. While challenges remain, the early success of pembrolizumab in shrinking tumors and stabilizing disease progression offers hope to patients who previously had limited options.