Endometriosis is a chronic and often painful condition that affects millions of women around the world. It occurs when tissue similar to the lining of the uterus (endometrium) grows outside the uterus, leading to various health issues, including pelvic pain and infertility. While it may be common, many women experience difficulty in getting diagnosed, and its impact on daily life can be significant. In this article, we will explore the symptoms, risk factors, and available treatment options for managing endometriosis, offering valuable information for women and healthcare professionals.
Table of Contents
- Introduction: What is Endometriosis?
- Symptoms of Endometriosis
- 2.1 Pelvic Pain
- 2.2 Heavy Menstrual Periods
- 2.3 Pain During Intercourse
- 2.4 Infertility
- Risk Factors for Endometriosis
- 3.1 Genetics
- 3.2 Age and Menstrual History
- 3.3 Immune System Disorders
- Diagnosis of Endometriosis
- Treatment Approaches for Endometriosis
- 5.1 Medications
- 5.2 Surgical Treatments
- 5.3 Lifestyle Changes
- 5.4 Fertility Treatments
- Living with Endometriosis: Coping and Support
- Conclusion: Managing Endometriosis for a Better Quality of Life
Introduction: What is Endometriosis?
Endometriosis is a medical condition where tissue similar to the lining inside the uterus (endometrium) starts to grow outside the uterus. This tissue can be found on the ovaries, fallopian tubes, and other organs in the pelvic cavity. During a woman’s menstrual cycle, the endometrial tissue normally thickens, breaks down, and sheds. However, when this tissue grows outside the uterus, it has nowhere to go, causing inflammation, scarring, and adhesions, leading to pain and other complications.
Although endometriosis is often associated with pelvic pain and infertility, it can affect other aspects of a woman’s health, leading to emotional distress and physical discomfort. It is a chronic condition, but with appropriate management, women can experience relief and maintain a high quality of life.
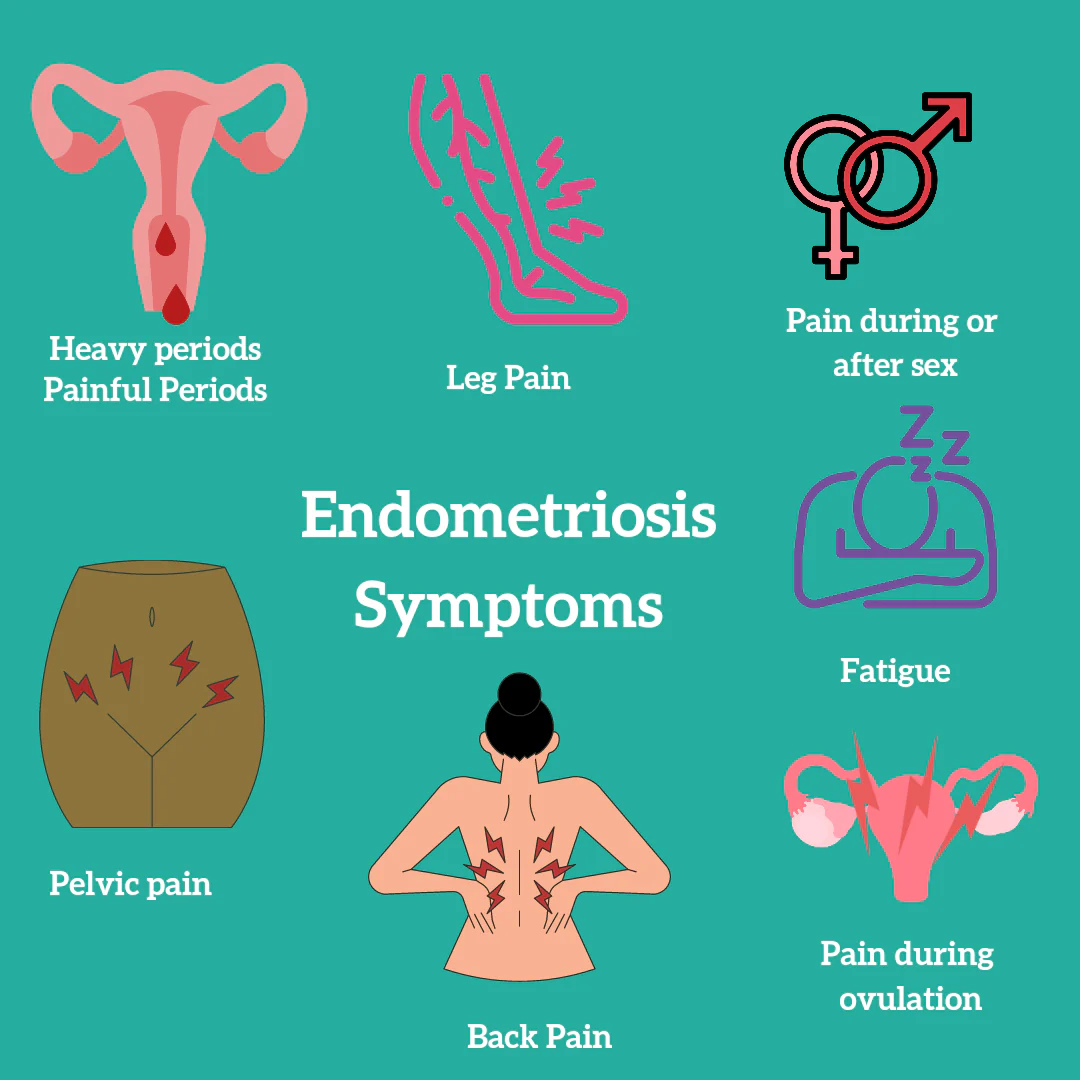
Symptoms of Endometriosis
Endometriosis can present with a variety of symptoms, ranging from mild to severe. While the intensity of symptoms varies from woman to woman, some of the most common signs to watch for include:
2.1 Pelvic Pain
Pelvic pain is one of the hallmark symptoms of endometriosis. It often coincides with menstruation and can be severe, lasting longer than typical menstrual cramps. Women with endometriosis may experience chronic pelvic pain, and this pain may worsen over time. Some report deep, stabbing pain during or after intercourse or during bowel movements.
2.2 Heavy Menstrual Periods
Women with endometriosis often experience heavy, prolonged menstrual bleeding. This symptom is known as menorrhagia. The increased bleeding may be accompanied by blood clots and may be so severe that it interferes with daily activities.
2.3 Pain During Intercourse
Pain during intercourse (dyspareunia) is another common symptom of endometriosis. This pain can range from mild discomfort to severe, deep pain, particularly during or after penetration. Women with endometriosis may find it difficult to enjoy intimate relationships due to this discomfort.
2.4 Infertility
Endometriosis can be a significant cause of infertility. It is estimated that 30-50% of women with endometriosis experience difficulty getting pregnant. The condition can interfere with the normal function of the ovaries, fallopian tubes, and uterus, making conception more challenging. Women who are having trouble conceiving should consult a healthcare provider to rule out endometriosis as a potential cause.
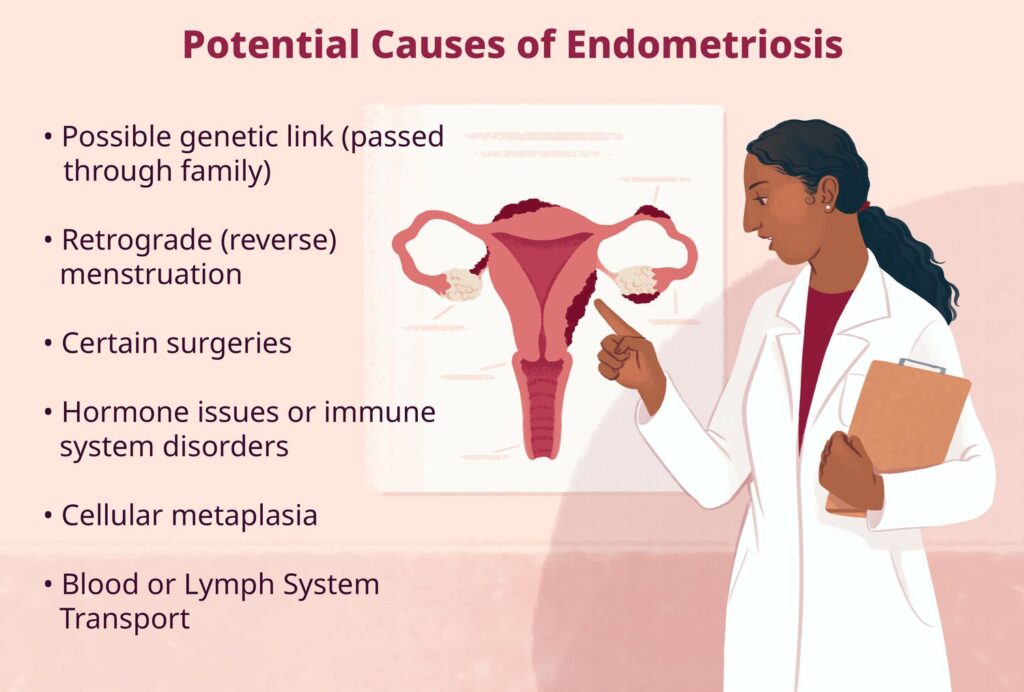
Risk Factors for Endometriosis
Although the exact cause of endometriosis remains unclear, several risk factors may increase a woman’s likelihood of developing the condition. Below are some of the main risk factors associated with endometriosis:
3.1 Genetics
Genetics play a crucial role in the development of endometriosis. If a woman has a first-degree relative, such as a mother or sister, with endometriosis, her chances of developing the condition are higher. Research suggests that certain genetic markers may predispose women to endometriosis, but more studies are needed to identify specific genes involved.
3.2 Age and Menstrual History
Endometriosis is most commonly diagnosed in women between the ages of 25 and 40. Women who have started their periods at an early age (before 12 years old) or have longer menstrual cycles are at a higher risk of developing the condition. Additionally, women who have fewer pregnancies or who experience delayed childbearing may be more likely to develop endometriosis.
3.3 Immune System Disorders
Certain immune system disorders, such as autoimmune diseases, may increase the risk of developing endometriosis. Some research suggests that women with conditions like lupus or Crohn’s disease may be more likely to develop endometriosis, potentially due to an underlying immune system dysfunction.
Diagnosis of Endometriosis
Diagnosing endometriosis can be challenging because its symptoms often overlap with other conditions, such as irritable bowel syndrome (IBS) or pelvic inflammatory disease (PID). The diagnostic process typically involves:
- Physical examination: A pelvic exam may reveal abnormalities or cysts that suggest endometriosis, although it cannot definitively diagnose the condition.
- Ultrasound or MRI: Imaging tests can be used to detect cysts or masses associated with endometriosis, although they cannot provide a complete diagnosis.
- Laparoscopy: The gold standard for diagnosing endometriosis is laparoscopy, a minimally invasive surgical procedure in which a small camera is inserted into the pelvic cavity. This allows the doctor to directly view and biopsy any endometrial tissue outside the uterus.
Treatment Approaches for Endometriosis
While there is no cure for endometriosis, several treatment options can help manage symptoms and improve quality of life. The appropriate treatment depends on the severity of the condition, symptoms, and whether the woman desires pregnancy.
5.1 Medications
Medications are often the first line of treatment for managing pain and other symptoms associated with endometriosis. Common medications include:
- Pain relievers: Over-the-counter medications, such as ibuprofen or naproxen, can help alleviate mild to moderate pain.
- Hormonal therapies: Hormonal treatments, such as birth control pills, patches, or intrauterine devices (IUDs), can regulate or stop menstruation and reduce the growth of endometrial tissue.
- Gonadotropin-releasing hormone (GnRH) agonists: These medications reduce estrogen production and induce a temporary state of menopause, helping to shrink endometrial lesions.
5.2 Surgical Treatments
In severe cases of endometriosis or when medications fail to provide relief, surgery may be necessary. Surgical options include:
- Laparoscopic surgery: A minimally invasive procedure to remove endometrial tissue, adhesions, and cysts.
- Hysterectomy: In cases where endometriosis has not responded to other treatments, a hysterectomy (removal of the uterus) may be recommended, especially if the woman does not desire future pregnancies.
5.3 Lifestyle Changes
Certain lifestyle changes can help manage endometriosis symptoms and improve overall health, including:
- Exercise: Regular physical activity can help reduce inflammation and improve blood circulation, which may alleviate pain.
- Diet: A diet rich in fruits, vegetables, whole grains, and lean proteins can support overall health. Some studies suggest that reducing red meat intake and incorporating anti-inflammatory foods, such as omega-3 fatty acids, may help alleviate symptoms.
- Stress management: Stress can exacerbate pain and inflammation, so practices like yoga, meditation, and mindfulness can be beneficial for managing symptoms.
5.4 Fertility Treatments
For women with endometriosis who are struggling with infertility, fertility treatments such as in vitro fertilization (IVF) may be recommended. IVF can help bypass any barriers caused by endometriosis, improving the chances of conception.
Living with Endometriosis: Coping and Support
Living with endometriosis can be physically and emotionally challenging. Women may experience frustration due to the unpredictability of symptoms, especially when trying to manage work, family, and social obligations. Coping strategies for managing the condition include:
- Support groups: Connecting with others who are experiencing similar challenges can offer emotional support and practical advice.
- Counseling or therapy: Professional support from a therapist or counselor can help women cope with the emotional toll of endometriosis, especially if they are dealing with infertility or chronic pain.
- Communication with healthcare providers: Open communication with doctors is essential for finding the most effective treatment plan and adjusting it as needed.
Conclusion: Managing Endometriosis for a Better Quality of Life
Endometriosis is a complex condition that can have a significant impact on a woman’s physical and emotional health. However, with the right treatment approach, including medications, surgery, lifestyle changes, and support, women can manage their symptoms and lead fulfilling lives. Early diagnosis and proactive management are crucial for reducing the impact of the condition and improving the chances of conception for women facing infertility.
If you suspect you have endometriosis or experience any of the common symptoms, consult with a healthcare provider for a proper diagnosis and treatment plan. With the right support, it is possible to manage endometriosis effectively and maintain a healthy and active lifestyle.