Osteoarthritis (OA) is the most common form of arthritis, affecting millions of people worldwide. It is a degenerative joint disease that can cause pain, stiffness, and loss of function, leading to reduced quality of life. While OA primarily affects older adults, younger individuals can also develop the condition, especially if they have risk factors like obesity, joint injuries, or family history.
In this article, we will explore the causes, symptoms, and latest treatment options for osteoarthritis. Whether you’re dealing with OA or seeking information to help a loved one, this guide provides a comprehensive look at how to manage this chronic condition and protect joint health.
Table of Contents
- Introduction: What is Osteoarthritis?
- Causes of Osteoarthritis
- Symptoms of Osteoarthritis
- Diagnosing Osteoarthritis
- Latest Treatment Options for Osteoarthritis
- Living with Osteoarthritis: Coping Strategies
- Conclusion: Managing Osteoarthritis for Better Joint Health

Introduction: What is Osteoarthritis?
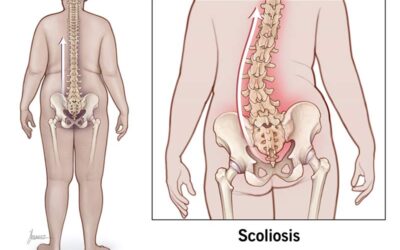
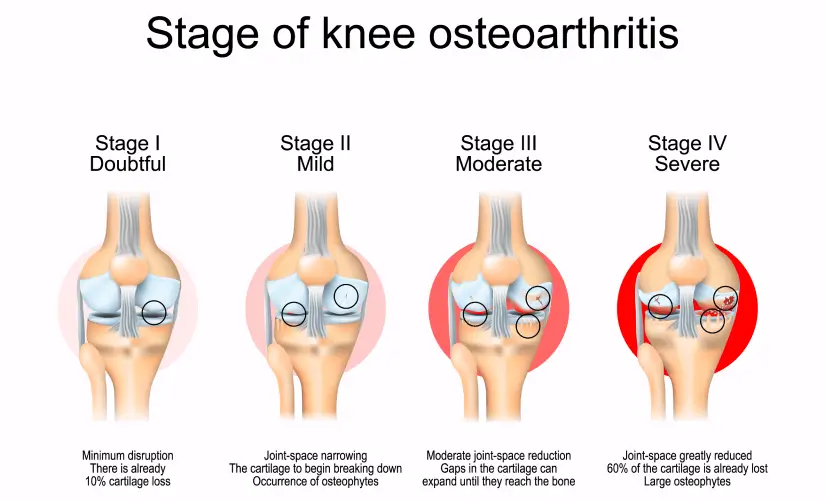
Osteoarthritis (OA) is a degenerative joint disease characterized by the breakdown of cartilage in the joints, which act as cushions between bones. As the cartilage wears away, bones begin to rub against each other, leading to pain, swelling, and stiffness. Over time, this can result in decreased mobility and, in severe cases, joint deformity.
OA most commonly affects weight-bearing joints, such as the knees, hips, and spine, but it can also impact the hands and other joints. Unlike inflammatory forms of arthritis (like rheumatoid arthritis), osteoarthritis is primarily a mechanical wear-and-tear condition.
Although there is no cure for OA, early diagnosis, lifestyle changes, and treatments can help manage symptoms, slow disease progression, and improve joint function.
Causes of Osteoarthritis
Osteoarthritis is a multifactorial disease, meaning several factors contribute to its development. Understanding the root causes of OA can help prevent or manage the disease more effectively.
2.1 Aging and Wear and Tear
The primary risk factor for osteoarthritis is aging. As we get older, the cartilage in our joints naturally wears down due to years of use. This “wear and tear” process is a gradual breakdown that occurs over time, leading to the onset of OA. While the disease is more common in individuals over 50, it can begin earlier in people with specific risk factors.
2.2 Genetic Factors
Genetics also play a role in the development of osteoarthritis. Research has shown that certain gene variations can increase susceptibility to OA, particularly in weight-bearing joints like the knees and hips. If a close family member has OA, there may be a higher risk of developing the condition.
2.3 Obesity and Joint Stress
Excess weight puts additional stress on weight-bearing joints, particularly the knees and hips, accelerating cartilage breakdown and increasing the risk of osteoarthritis. Obesity is one of the most significant modifiable risk factors for OA. Losing weight through diet and exercise can help relieve joint pressure and reduce the risk of developing OA or slow its progression.
2.4 Injuries and Previous Joint Damage
Joint injuries, such as those sustained in sports or accidents, can also increase the likelihood of developing osteoarthritis. Injuries to ligaments, cartilage, or bones can lead to abnormal joint mechanics, which increase stress on the cartilage and eventually lead to OA. Even if the injury heals, the affected joint is more susceptible to future degeneration.
Symptoms of Osteoarthritis
Osteoarthritis symptoms can vary depending on the severity of the disease and the affected joints. Common symptoms include:
3.1 Pain and Stiffness
The most prominent symptom of osteoarthritis is joint pain, particularly after prolonged activity or at the end of the day. The pain may be mild at first but can intensify as the cartilage deteriorates. Stiffness, especially after resting or upon waking, is also a hallmark of OA.
3.2 Swelling and Tenderness
Inflammation may occur around the affected joint, causing visible swelling. The joint may feel tender to the touch, and movement may exacerbate discomfort.
3.3 Decreased Range of Motion
As OA progresses, the affected joint may lose its flexibility and range of motion. This can make it difficult to perform daily activities such as walking, climbing stairs, or reaching for objects.
Diagnosing Osteoarthritis
To diagnose osteoarthritis, healthcare providers conduct a thorough physical examination, review the patient’s medical history, and may recommend imaging tests. Common diagnostic tools include:
- X-rays: X-rays help visualize joint damage, including bone spurs (osteophytes) and cartilage loss.
- MRI: Magnetic resonance imaging (MRI) provides detailed images of the soft tissues, including cartilage, and can reveal the extent of joint damage.
- Joint Fluid Analysis: In some cases, a joint aspiration (removal of fluid from the joint) may be performed to rule out other conditions, such as gout or infection.
Latest Treatment Options for Osteoarthritis
While there is no cure for osteoarthritis, a combination of medications, therapies, and lifestyle changes can help manage symptoms and improve joint function.
5.1 Medications for Osteoarthritis
Medications are often the first line of treatment for managing osteoarthritis symptoms. Common medications include:
- Pain Relievers: Over-the-counter (OTC) pain relievers, such as acetaminophen (Tylenol), help reduce pain and discomfort.
- Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): Drugs like ibuprofen (Advil) and naproxen (Aleve) reduce inflammation and alleviate pain.
- Corticosteroid Injections: In cases of severe pain, corticosteroid injections into the joint can provide temporary relief by reducing inflammation.
- Topical Analgesics: Creams, gels, or ointments applied to the skin can also help relieve joint pain, especially in the hands or knees.
5.2 Physical Therapy and Exercise
Physical therapy is crucial for improving joint function, strength, and flexibility. A physical therapist can develop a personalized exercise plan to strengthen muscles around the affected joint, which helps to support and protect the joint. Regular low-impact exercises such as swimming, walking, or cycling can improve mobility and reduce stiffness.
5.3 Injections and Surgical Interventions
In some cases, treatments such as joint injections or surgery may be necessary:
- Hyaluronic Acid Injections: These injections help lubricate the joint, reducing friction and providing pain relief.
- Joint Replacement Surgery: In severe cases of OA, especially in the hips or knees, joint replacement surgery (e.g., knee or hip replacement) may be recommended to restore joint function and improve mobility.
5.4 Emerging Therapies: Stem Cell Treatment and Platelet-Rich Plasma (PRP)
Emerging treatments like stem cell therapy and platelet-rich plasma (PRP) injections are being explored as potential options for OA management. Stem cell therapy aims to regenerate damaged cartilage, while PRP therapy uses the patient’s own blood platelets to promote healing and reduce inflammation in the affected joints.
While these therapies are still being studied, early results have shown promise in reducing pain and improving joint health.
Living with Osteoarthritis: Coping Strategies
Living with osteoarthritis requires a holistic approach to managing pain and maintaining an active lifestyle. Some strategies include:
- Weight Management: Losing weight reduces the strain on weight-bearing joints, slowing the progression of OA.
- Assistive Devices: Tools such as braces, canes, or specially designed shoes can provide extra support and ease joint strain.
- Joint Protection: Avoiding repetitive movements, taking breaks, and using ergonomic tools can reduce the risk of joint stress.
Conclusion: Managing Osteoarthritis for Better Joint Health
Osteoarthritis is a progressive condition that can significantly impact your daily life, but with the right approach, its symptoms can be managed effectively. Understanding the causes, recognizing early symptoms, and seeking timely treatment can help protect