Introduction
The development of antimicrobial resistance stands as one of the major worldwide healthcare challenges during the current century.
The environmental domain represents a primary source of antimicrobial resistance development while healthcare facilities have historically received most attention for antibiotic-related issues.
AMR develops through various complex mechanisms in which environmental factors contribute to antibiotic resistance and resistance to other antimicrobial agents.
This study explores different environmental factors behind antimicrobial resistance growth while presenting strategies to reduce its effects.

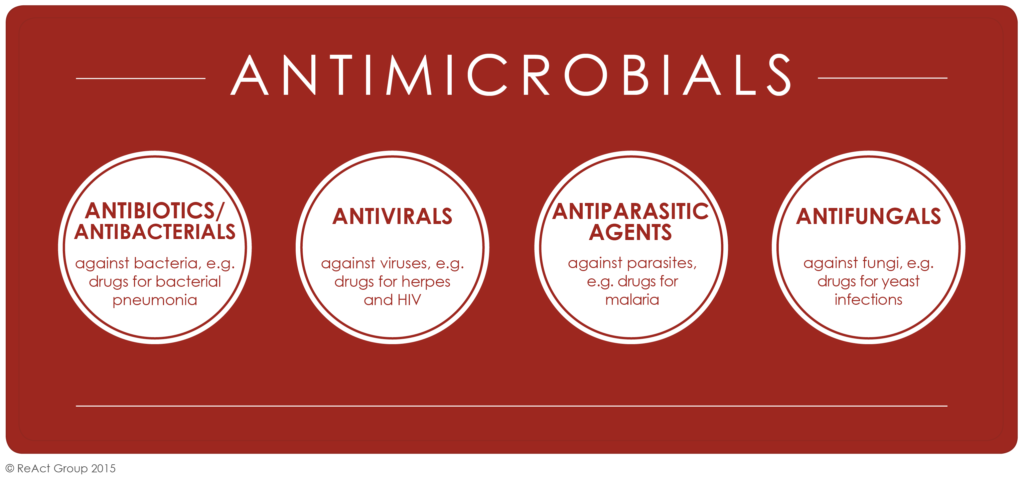
What is Antimicrobial Resistance (AMR)?
The resistance displayed by microorganisms such as bacteria and viruses and fungi and parasites against medicinal substances used in infection treatment constitutes antimicrobial resistance.
Conditions that cause bacteria to become resistant to antibiotic treatments have the effect of making standard medical treatments ineffective causing extended hospital stays and more deaths together with elevated medical expenses.
The environment facilitates the movement of resistance-bearing microbes between sources while healthcare centers and agricultural operations drive the development of AMR through their improper antibiotic applications.
How the Environment Contributes to AMR
Antimicrobial-resistant bacteria and their genes find a significant reservoir for transmission within the environment. AMR finds pathways through the environment from the combination of agricultural runoff together with wastewater discharge and medical waste contamination. The following environmental elements are responsible for spreading AMR:
🔘 Agricultural Practices Environmental
contamination with antimicrobial-resistant bacteria emerges mainly from agricultural activities. The extensive administraton of antibiotics during farming processes leads to AMR development through these key mechanisms:
In livestock management practices farmers frequently offer animals antibiotic drugs both to support development and stop sickness conditions using minimal strength medications.
Sub-therapeutic antimicrobial doses serve as a survival advantage for resistant bacteria as they do not eliminate bacteria yet enable their multiplication and this bacterial transfer occurs from animals to humans through meat consumption or animal contact.
Farmers implement antibiotic pesticides as antimicrobial agents as a disease prevention measure in agricultural agriculture. These chemical substances penetrate into soil while entering water systems then modify microbial communities before creating resistant agents.
The drainage from agricultural fields delivers resistant bacteria into liquid water resources including rivers and lakes and the subterranean water system thus advancing resistance evolution.
🔘 Wastewater and Sewage Contamination
Hospitals together with industrial facilities and residential areas release wastewater that contains major amounts of antimicrobial agents and resistant bacteria.
Unprocessed wastewater treatment systems allow resistant organisms to pass into natural water reservoirs. The environmental release of wastewater poses a critical issue since wastewater treatment facilities commonly fail to eliminate antibiotics and other chemicals before their complete removal.
This issue is most prominent in cities where treatment facilities do not manage to remove all contaminants. The absence of functional waste management systems in developing nations causes environmental pollution since raw sewage frequently pollutes local water sources.
The environmental spread of AMR occurs through the process which subsequently leads to infection transmission between community members.
🔘 Environmental Reservoirs of Resistant Bacteria
The environment maintains ability to serve as a storage site for resistant bacteria. Any of the three environmental elements including soil, water and air can serve as hosts to bacteria that display acquired resistance characteristics.
Resistant bacteria transfer from environment to humans and animals by touching infected items and by eating contaminated food or drinking polluted water.
The long-term survival of resistant bacteria in the environment drives the continuous spread of AMR. Many environmental reservoirs that carry resistant bacteria exist in human activity areas such as cities and agricultural zones thus facilitating an increased transmission of resistant microorganisms.
4. The Impact of Antimicrobial Resistance on Public Health
- Environmental factors in antimicrobial resistance development cause severe effects to public health. When environment-friendly bacteria multiply beyond control they create numerous infections which are challenging or even impossible to cure with current antibiotic treatments.
- The consequences of AMR include: Such infections from resistant bacteria become more challenging to manage through medication which needs advanced expensive treatment.
- Vulnerable patient groups who embody the elderly along with people with impaired immune systems face greater mortality and morbidity risk because of antibiotic resistance.
- The healthcare stay of patients with resistant infections extends due to treatment delays therefore producing more contact with antibiotic-resistant microorganisms.
- The spread of AMR generates substantial financial expenses for healthcare systems because patients need longer medication treatment periods and specialized medications while requiring intensive medical services.
- Effective medical treatment including surgeries and cancer management and organ transplants depends fully on antibiotic efficacy.
- The increasing number of antimicrobial-resistant infections damages the current medical progress and exposes numerous patients to severe risks.

The Role of Environmental Policy in Combating AMR
- Control of antimicrobial resistance through the environment needs comprehensive environmental policies and regulatory mechanisms. Some key policy approaches include: Governments should enact regulations to control the excessive antibiotic use both in livestock farming and crop cultivation systems.
- The government should establish a policy to control antibiotic usage for growth promotion alongside restrictions on veterinary antibiotics sales together with an encouragement for probiotics usage.
- The government along with industries must dedicate funds to improve wastewater treatment centers which remove antimicrobial agents more effectively before releasing pollutants to the environment.
- Staff must focus on two main areas: first they should enhance pipe systems and research better filtration solutions while secondly they must maintain strict wastewater regulations.
- The issue of antimicrobial resistance demands worldwide unity among nations because it affects every country. The reduction of resistant pathogen environmental spread demands unified action between public organizations and the private sector under governmental supervision through policy and strategy coordination and information sharing.
Several critical actions exist to decrease the environmental risk associated with antimicrobial resistance.
| ⚫ A diverse set of measures needs implementation for cutting environmental factors contributing to antimicrobial resistance. The required solutions operate in multiple economic areas including healthcare as well as agriculture and need active multi-faceted engagements from local to national to international levels. |
| ⚫ Improving Wastewater Treatment The primary way to combat environmental AMR development rests in enhancing wastewater treatment systems. This includes: Adopting novel filtration methods like membrane solutions together with activated sludge processes and ozonation would enhance wastewater surgery to eliminate antibiotics and resistant bacterial components. The implementation of decentralized wastewater treatment systems installed across rural regions helps minimize antimicrobial agent emissions to the environment. The correct handling of surplus pharmaceutical products through proper disposal stands as a method to avoid antimicrobial agent contamination of water supplies. |
| ⚫ Sustainable Agriculture Practices Farmers should put into practice environmentally friendly farm management techniques which minimize both the necessity of antibiotic consumption and the development of microbial resistance. These practices include: Antibiotic use in livestock production should be restricted to medical treatment alone since this practice decreases pressure that selects antibiotic-resistant bacteria. Crop Rotation together with Integrated Pest Management decreases the requirement for both chemical pesticides and antimicrobial agents during crop production. |
| ⚫ Enhanced Surveillance and Monitoring Organizations together with governments need to make environmental resistant bacteria and antimicrobial agent monitoring their top priority. Surveillance programs detect locations with resistance outbreaks as well as evaluate the impact of implemented monitoring approaches. Key steps include: Regular water quality checks that verify antimicrobial agents and resistant bacteria help multiple them during early stages of contamination. National surveys of resistant bacteria being maintained in environmental sources provide indications for developing specific intervention programs and regulatory frameworks. |
Conclusion
Antimicrobial resistance from environmental sources continues to increase at an alarming rate so immediate government-intervention and industry involvement and public participation become necessary.
Agricultural practices together with wastewater contamination make the environment a primary facilitator of resistant bacteria spread.
The fight against acquired microbial resistance requires complete solutions that combat environmental factors which cause bacterial resistance.