Introduction
Hospital-acquired Pseudomona infections represent an escalating global health problem due to antibiotic-resistant bacteria. Among antibacterial pathogens this aeruginosa stands out as the most threatening to hospital environments.
The pathogenic bacterium causes diverse infections which range in severity from minor ones to dangerous conditions yet remains tough to treat due to its speedy development of resistance against multiple antibiotics.

This article investigates the increasing number of Pseudomonas infections acquired in hospitals as well as their effects on healthcare systems and the expanding problem of drug-resistant bacteria.
What is Pseudomonas Aeruginosa?
The bacterial species Pseudomonas aeruginosa exists among numerous environments while it colonizes both soil and water as well as hospital environments.
Hospital environments become ideal breeding grounds for this because it has the survival capability to persist on medical equipment along with surfaces and moist spaces including sinks and showers.
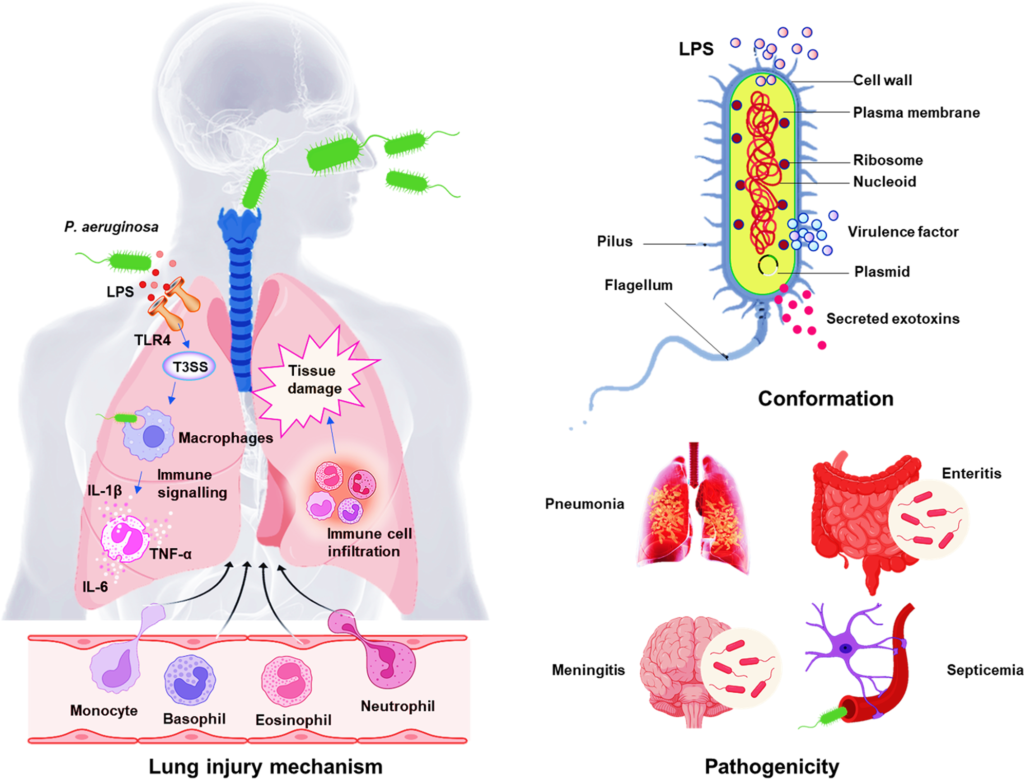
This bacterium leads to diverse types of diseases that strongly affect patients whose immune system becomes weak because of surgical procedures and cancer treatment or organ transplant.
This bacterium causes infections of pneumonia bloodstream and urinary tract issues as well as wound infections. The high danger level of this aeruginosa originates from its native ability to withstand multiple antibiotics commonly prescribed by doctors.
Healthcare professionals throughout the world have made hospital-acquired Pseudomonas infections their primary clinical concern.
Hospital-Generated Pseudomonas Infections
Hospital personnel introduce Pseudomonas aeruginosa through various contaminated medical equipment that includes catheters together with ventilators and intravenous lines.
Medical procedures which penetrate natural body defenses through intubation or surgery create invasion points that enable this to penetrate bodily tissues and produce infections.
The perfect conditions for this survival exist within hospitals because of multiple existing conditions such as: The excessive administration of antibiotics in healthcare facilities creates survival conditions that select resistant bacteria strains.
People with weakened immune systems among those receiving chemotherapy or who have chronic illnesses or those undergoing major surgeries are at increased risk for developing infections during healthcare settings.
Medical equipment used within high-risk areas which are not correctly sterilized presents opportunities for this spread.
Bacteria will spread quickly in hospitals when healthcare institutions fail to implement proper hygiene and sterilization protocols.
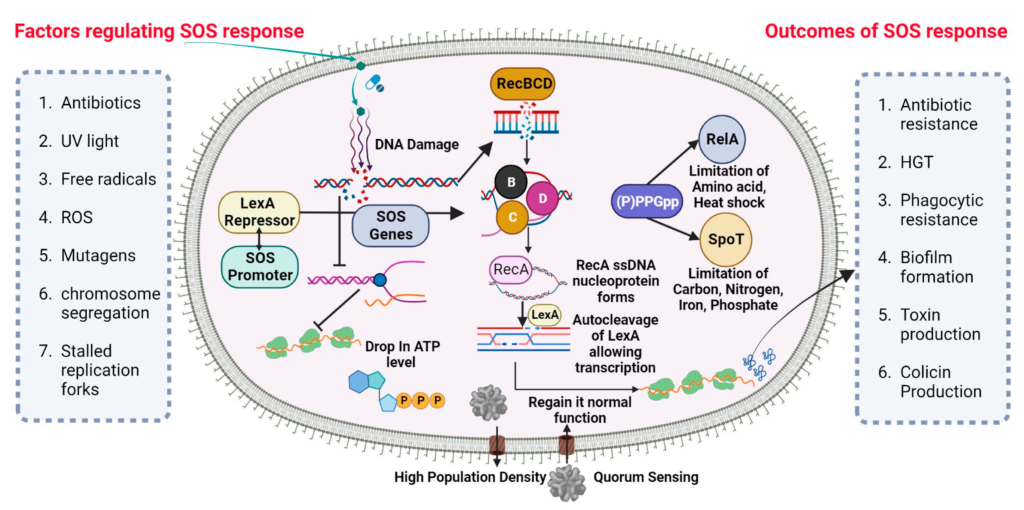
The Role of Antibiotic Resistance in Pseudomonas
Infections Bacteria adapt resistant mechanisms against drugs which previously eliminated them or stopped their multiplication processes.
The antibiotic-resistant capabilities of this aeruginosa make it difficult to treat this bacterium because it develops resistance against multiple classes of antibiotics.
Several ensemble factors contribute to bacterial resistance of antibiotics. Through use of active efflux pumps Pseudomonas successfully moves antibiotics out of its bacterial cell prior to drug effectiveness.
Bacterium releases the β-lactamase enzyme and other enzymes that break down penicillin as well as cephalosporin antibiotics. This forms biofilms through the production of protective bacterial clusters known as biofilms.
The bacterial biofilm acts as defense against both immune system responses and antibiotic treatment. The bacterium gains resistance to particular antibiotics through its natural ability for genetic mutation.
Hospital-acquired this infections are becoming harder to treat because health facilities house patients who face elevated risk levels.
Multidrug-resistant (MDR) this strains have emerged because both situations have evolved into a serious issue because they resist multiple antibiotic classes.
The Impact of Hospital-Acquired Pseudomonas Infections
Hospital-acquired infections from Pseudomonas aeruginosa create extensive medical consequences that affect patients together with hospital management systems. Infections from Pseudomonas lead to the need for extended hospital time with higher spending on health care and raise death rates.
Hospital patients having Pseudomonas infections need advanced therapeutic approaches using broad-spectrum antibiotics leading to intensified treatment risks.
Hospital-acquired this infections cause several critical health problems to appear. Hospitalized patients who develop Pseudomonas infections spend longer periods in medical facilities because of this condition which creates excessive strain on available healthcare resources while raising total healthcare bills.
The pathogenic nature of this infections causes fatal results in immunocompromised patients when proper medical care does not treat the condition.
The therapy of resistant Pseudomonas strains requires healthcare providers to administerxitin and carbapenem antibiotics as their final treatment options.
The practice of using antibiotic medications leads to the emergence of novel antibiotic resistance. Healthcare workers who treat infected patients face high risks of contracting the infection because insufficient infection control procedures in their workplace.
The Challenge of Antibiotic Resistance in Pseudomonas
Drugs-resistant Pseudomonas aeruginosa creates significant difficulties for physicians who practice medicine. Treatment options for healthcare providers become restricted because of resistance along with an increased probability for failed treatment results.
These elements play leading roles in increasing this issue: The combination of improper antibiotic prescriptions for non-bacterial infections with incomplete medication completion facilitates antibiotic resistance development. Hospital antibiotic usage during prophylactic and empiric treatment situations contributes to the problem.
The production of new antibiotics has experienced a declining pace throughout the last decades because drug development requires significant expenses and extensive complexity.
Treatment options for resistant infections become harder to obtain because of the reduced availability of therapeutic options. Through globalization medical operations including patient mobility together with healthcare staff and hospital visitors support Pseudomonas resistant strain transfer from hospital to hospital across worldwide networks.
Pseudomonas organisms endure in environmental conditions persistently especially when moisture is present. The pathogen finds suitable conditions to reproduce when it infects water supplies or sinks or medical equipment which creates additional risks of transmission between healthcare practitioners.
Preventing Hospital-Generated Pseudomonas
Infections Multidirectional prevention of Pseudomonas hospital infections must combine healthcare practices that protect against transmission with antibiotic surveillance methods along with environmental cleaning protocols.
The reduction of Pseudomonas hospital infection spread requires implementing these strategies: Hospital infection control depends on three main factors: maintaining proper hand hygiene and applying routine hospital surface cleaning together with medical equipment sterilization protocols.
Hospital programs for antibiotic stewardship help prevent the occurrence of antibiotic resistance by promoting proper antibiotic administration.
Medical facilities should maintain continual Pseudomonas infection and antibiotic resistance pattern monitoring as this approach enables quick outbreak detection for healthcare teams.
Healthcare staff must teach patients about proper hand hygiene techniques as well as adhere to infection prevention methods which decreases the chance of hospital-acquired infections.
New antibiotic development combined with researcher investigation of alternative treatments and vaccine development represents an essential approach to combat antibiotic-resistant Pseudomonas infections.
Conclusion
Healthcare facilities face a major expanding issue due to Pseudomonas infections produced inside hospitals that display antibiotic resistance.
This pathogen remains an extensive challenge to healthcare providers and public health infrastructures because it continues to develop new adaptive characteristics.
The successful resolution of this problem demands joint work between organizations which combines advanced infection prevention practices and antibiotic stewardship initiatives and new treatment development funding.
Multiple prevention measures will help reduce Pseudomonas aeruginosa’s dangerous potential so healthcare facilities remain secure for patients and medical staff alike.
Hospital-acquired infections will continue to endanger vulnerable patients so the global health community needs individual and institutional actions and awareness to stop this threat.


